In-Vitro USP 87 Vs. In-Vivo USP 88 Cytotoxicity Testing
What is cytotoxicity?
Cytotoxicity refers to molecules and compounds that are poisonous to living cells. Cytotoxins are often chemical but can also be from natural or biological sources.
What is cytotoxicity testing?
Cytotoxicity testing evaluates the biological reactivity of mammalian cells and tissues to contact with elastomeric plastics, excipients, and other materials that will come in direct or indirect patient contact during medical product use. Thus, sometimes cytotoxicity testing is referred to as biological reactivity testing. Cytotoxicity is significant as it evaluates the biological effects of a sample’s leachable chemicals. The types of cytotoxicity testing to perform for your medical device or product depend upon the final product, the final product’s intended use, and the materials the final product is made of and packaged within.
How are cytotoxicity tests performed?
Most plastics (polymers) used for injectable, parenteral, and medical products will only require in-vitro cytotoxicity testing covered by USP 87. However, if material components do not meet the requirements of USP 87 direct contact, agar diffusion, and elution testing, in-vivo cytotoxicity testing outlined in USP 88 will be needed. The required in-vivo testing will be implantation, intracutaneous injection, or systemic injection tests. A description of all in-vitro and in-vivo cytotoxicity tests is provided below.
In-Vitro Cytotoxicity Testing (USP 87)
In-vitro tests are required to determine the biological reactivity of mammalian cells to contact with elastomeric plastics and other polymeric materials. Three in-vitro cytotoxicity tests are used to assess systemic biological reactivity. These tests are direct contact, agar diffusion, and elution assays.
What is in-vitro direct contact testing?
Direct contact cytotoxicity tests can evaluate nearly all materials. Additionally, sample extraction and testing of a sample’s leachable chemicals can coincide with direct contact testing. Direct contact methods cannot assess very low density or extremely high-density materials that could cause mechanical damage to cultured live cells.
What is in-vitro agar diffusion testing?
Agar diffusion tests are beneficial for assessing the cytotoxicity of elastomeric closures. In these tests, the agar layer acts as a cushion. The agar protects the cells from any mechanical damage and allows leachable chemicals to diffuse from the product or packaging samples. The cells are then evaluated to determine the toxicity of the samples. Material extracts can also be assessed for cytotoxicity using the agar diffusion test by applying material extracts to a piece of filter paper.
What is in-vitro elution testing?
Elution tests are designed for evaluating extracts from plastic materials. Elution tests for cytotoxicity are beneficial for assessing high-density materials and evaluating dose-response in-vitro. Elution testing methods allow sample extraction to occur multiple times and under various temperature conditions.
How are direct contact tests performed?
Sample pieces with flat surfaces of at least 100 square millimeters (mm) are prepared for direct contact testing. Polyurethane film with zinc (ZDEC2 or ZDBC) is used as a positive control. Next, L-929 mammalian fibroblast cells are grown in a serum-supplemented minimum essential medium (MEM), and a cell suspension is prepared. Equal amounts of the L-929 cell suspension are added to culture plates with a 35 mm diameter to create a single layer cell culture. After L-929 cells have been cultured to reach the appropriate confluence, the cell culture medium is aspirated from the plates and replaced with a fresh culture medium. Next, a single item (i.e., product sample, positive control, or negative control) is placed in each 35 mm culture dish. All samples and controls are cultured in duplicate or triplicate at 37 ± 1°C in a humidified incubator containing 5 ± 1% carbon dioxide.
After incubation, each sample, positive control, and negative control are examined under a microscope. In some cases, cells are stained to support assessing biological reactivity. The biological reactivity of the cells exposed to the sample or sample extracts is rated on a scale of 0-4 (see here for details). The biological reactivity is determined by assessing the nonlethal injury of the cells (cellular degeneration) and any structural defects (malformations) the cells have. The direct contact test is valid if the observed responses to the negative controls are grade 0 and the Positive controls are all at least grade 3. The sample meets the requirements of the direct contact test if the biological responses of the samples are not greater than grade 2.
How are agar diffusion tests performed?
For agar diffusion testing, materials or medical device extracts are prepared using a 0.9% sodium chloride injection or a mammalian cell culture media. For samples that aren’t extracts, portions of the test samples with flat surfaces not less than 100 square millimeters (mm) in surface area are used for the agar diffusion assay. Polyurethane film with zinc (ZDEC2 or ZDBC) is used as a positive control.
Next, L-929 mammalian fibroblast cells are grown in a serum-supplemented minimum essential medium (MEM) to greater than 80% confluence. The culture medium is then aspirated, and a solution of not more than 2% agar is added to each 60 mm diameter plate. The agar layer must be thin enough to allow the diffusion of leached chemicals from the samples. Finally, samples, positive controls, and negative controls (or their extracts) are added on top of the solidified agar surface. All samples and controls are cultured in duplicate. Then all of the cultures are incubated at 37 ± 1°C in a humidified incubator containing 5 ± 1% of carbon dioxide.
After incubation, cells exposed to samples, positive controls, and negative controls are stained or evaluated without staining under the microscope. The biological reactivity of the cells exposed to the sample or sample extracts is rated on a scale of 0-4 (see here for details). The biological reactivity is determined by assessing the nonlethal injury of the cells (cellular degeneration) and any structural defects (malformations) the cells have. The agar diffusion test is valid if the observed responses to the negative controls are grade 0 and the positive controls are all at least grade 3. The sample meets the agar diffusion test’s requirements if the samples’ biological responses are not greater than grade 2.
How is elution testing performed?
For elution testing, product or material extracts are prepared using a 0.9% sodium chloride injection or mammalian cell culture media. Often 0.1 g of elastomeric materials or 0.2 g of other plastic material is used per milliliter of extraction medium. Polyurethane film with zinc (ZDEC2 or ZDBC) is used as a positive control.
Next, L-929 mammalian fibroblast cells are grown in a serum-supplemented minimum essential medium (MEM), and a cell suspension is prepared. Equal amounts of the L-929 cell suspension are added to culture plates with a 35-millimeter diameter to create a single-layer cell culture. After L-929 cells have been cultured to reach the appropriate confluence, the cell culture medium is aspirated from the plates and replaced with extracts from material samples, positive controls, and negative controls. Extracts from cell culture media remain without dilutions. Extracts prepared with the Sodium Chloride Injection are diluted to a 25% extract concentration with a serum-supplemented cell culture medium. All samples and controls are cultured in duplicate or triplicate at 37 ± 1°C in a humidified incubator containing 5 ± 1% carbon dioxide.
After incubation, cells exposed to samples, positive controls, and negative controls are stained or evaluated without staining under the microscope. The biological reactivity of the cells exposed to the sample or sample extracts is rated on a scale of 0-4 (see here for details). The biological reactivity is determined by assessing the nonlethal injury of the cells (cellular degeneration) and any structural defects (malformations) the cells have. The elution test is valid if the observed responses to the negative controls are grade 0 and the positive controls are all at least grade 3. The sample meets the elution test’s requirements if the samples’ biological responses are not greater than grade 2.

What are the differences between in-vitro direct contact, agar diffusion, and elution testing?
Direct contact tests evaluate medical devices, materials, or packaging sample pieces with flat surfaces not less than 100 square millimeters (mm). In contrast, elution tests assess the cytotoxicity of liquid extracts from sample pieces. Agar diffusion tests are best for evaluating elastomeric closures due to the utilization of an agarose layer for cytotoxicity testing. For all in-vitro test methods, L-929 fibroblast cells are used to evaluate cytotoxicity.
In-Vivo Cytotoxicity Testing (USP 88)
In-vivo tests are required in certain instances to determine the systemic biological reactivity of mammalian cells to contact with elastomeric plastics and other polymeric materials. The cytotoxicity tests performed for your medical device or product depend upon the final product’s packaging, intended use, and material construction. Three in-vivo cytotoxicity tests are used to assess systemic biological reactivity. These tests are implantation, intracutaneous injection, and systemic injection studies.
How is implantation cytotoxicity testing performed?
The implantation test is designed to evaluate the reaction of living tissue to polymers by implanting the device or therapeutic product into animal tissue. Material samples must be aseptically prepared and surgically placed under aseptic conditions to ensure accurate implantation results. The factors below should be considered and tested when evaluating the cytotoxicity of implanted polymers.
Factors that can impact the suitability of a material for its intended use are:
- Material composition
- Material processing and cleaning procedures
- Contacting media(s)
- Inks
- Adhesives
- Absorption properties
- Adsorption and permeability of preservatives
- Conditions of storage
The implantation tests are performed by surgically introducing a material sample under evaluation into a test animal. There are two forms of implantation testing, intramuscular implantation in rabbits and subcutaneous implantation in rats. Both implantation studies are described in further detail below.
Intramuscular Implantation In Rabbits
Intramuscular implantation testing uses healthy adult New Zealand rabbits. For intramuscular implantation, test specimens are placed into needles for implantation delivery. Materials with physical characteristics that prevent needle delivery should use the subcutaneous rat implantation model instead.
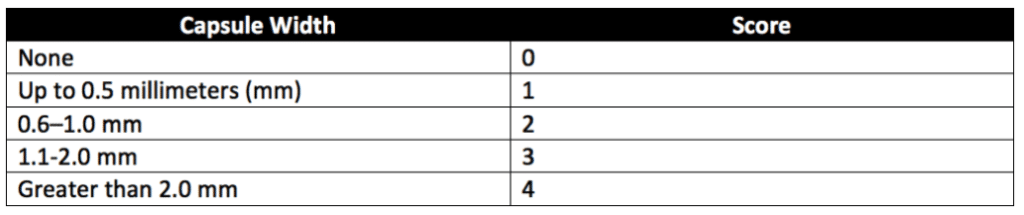
For product implantation, eight strips of the sample material and four USP-approved, high-density polyethylene RS strips are prepared. Each strip should measure not less than ten millimeters by one millimeter. To avoid hurting tissues upon implantation, the edges of the strips should be as smooth as possible. Each strip is implanted using a hypodermic needle (15–19 gauge) with an intravenous point and a sterile trocar. Strips are embedded by inserting the sanitary plastic strips into the hypodermic needle and then using the needle to implant the strips into the rabbits’ muscular tissues. Healthy adult rabbits weighing not less than 2.5 kilograms and with paravertebral muscles large enough for test strip implantation are used. Only paravertebral muscles are used for implantation sites. After the animals are anesthetized, the fur along the implantation areas of each animal is clipped. Then the implantation sites are cleaned. Next, four sample strips are implanted into the paravertebral muscle on one side of each of the two rabbits’ spines. Two strips of high-density polyethylene RS are embedded in the opposite paravertebral muscle of each animal as negative controls. Animals are exposed to the implanted strips for at least 5-days (120-hours) before tissue assessment. The tissue area surrounding the center of each implant strip is examined microscopically. Sample and control implant sites are assessed for hemorrhage, necrosis, discolorations, and infections. All observations are recorded, and encapsulation sites are measured to the nearest 0.1 millimeters. The scoring system in Table 1 below is used for tissue assessment. After all tissue scores are taken, differences between the average scores for the sample and control sites are calculated. Samples pass the implantation test if the calculated difference does not exceed 1.0 or if the difference between the sample and control mean scores for more than one of the four implant sites does not exceed 1 for any implanted animal.
Subcutaneous Implantation In Rats
For subcutaneous implantation in rats, ten samples and ten controls (USP high-density polyethylene RS) are prepared for the experiment. To avoid hurting tissues upon implantation, the edges of the sample and control strips should be as smooth as possible. Five healthy albino rats weighing 225–350 grams are used for testing. Implantation sites along the rat’s spinal columns are prepared similarly to the implantation sites for rabbits. The rats are anesthetized via AAALAC guidelines. After the initial incision, blunt dissection is used to separate the fascia connecting skin to muscle to form a pocket underneath the skin lateral to each side of the incision. A sterile sample is inserted into each tissue pocket, and the incision closed with wound clips or sutures. Two test samples and two control samples are implanted in each of the five rats. The animals are kept for at least seven days following sample implantation before tissues are assessed.
Similar to implantation in rabbits, the area of the tissue surrounding the center of each implant strip is examined microscopically. Sample and control implant sites are assessed for necrosis, hemorrhage, discolorations, and infections. All tissue observations are recorded, and encapsulation sites are measured. The scoring system in Table 1 (Table 6 of USP 88) is used for skin reaction assessment following surgical implantation in animals. After all tissue scores are taken, differences between the average scores for the sample and control sites are calculated. The implantation test is passed if the difference does not exceed 1.0 or if the difference between the sample and control mean scores for more than one of the four implant sites does not exceed 1 for any implanted animal.
What is in-vivo systemic injection testing for cytotoxicity?
A systemic injection is an injection into the circulatory system. Systemic injection testing determines the local biological responses of animals (mice) to plastic extracts injected into the bloodstream. Systemic injection testing and intracutaneous testing may be performed using the same extracts. Extracts are prepared depending on the heat resistance of the material being assessed. Thus, extracts are prepared at 50°, 70°, or 121°C. Natural elastomers are tested in sodium chloride injection and vegetable oils only. Sample sizes for elastomer extract preparations are twenty-five centimeters squared worth of combined surface area per twenty milliliters of extract medium. Elastomers used for extracts must remain uncut. USP 88 provides additional details on extract preparations for intracutaneous testing.
Systemically injected mice are assessed immediately after injection and at 4, 24, 48, and 72 hours after injection. Each study uses ten mice. All mice injected with polymer extracts must show the same or less reactivity as controls injected with blanks to pass this examination.
What is in-vivo intracutaneous testing for cytotoxicity?
An intracutaneous injection is an injection between the layers of the skin. Intracutaneous testing determines the local biological responses of animals (rabbits or guinea pigs) to plastic extracts injected under the skin. Systemic injection testing and intracutaneous testing may be performed using the same extracts. Extracts are prepared depending on the heat resistance of the material being assessed. Thus, extracts are prepared at either 50°, 70°, or 121°C. Natural elastomers are tested in sodium chloride injection and vegetable oils only. USP 88 provides additional details on extract preparations for intracutaneous testing.
For each plastic sample, two animals are intracutaneously injected. After injection, the injection sites are assessed for evidence of any tissue reaction such as erythema, edema, and necrosis. All animals are observed at 24, 48, and 72 hours after injection for tissue reaction. The average erythema and edema scores for the control injection sites are also assessed at 24, 48, and 72 hours. Scoring systems and pass/fail criteria for this test can be found in USP 88.
What are the differences between in-vivo implantation, intracutaneous injection, and systemic injection testing?
Unlike systemic injection and intracutaneous testing, implantation testing does not use product extracts for testing procedures. Instead, small pieces of the product or materials are directly implanted into rabbit or rat tissues for implantation testing. Implantable medical devices would likely undergo implantation cytotoxicity testing because implantation testing best models the product’s use in patients. Products that directly contact the circulatory system or are recirculating blood for a patient would undergo systemic injection testing because systemic injection better models the exposure level of the device with patient fluids. Intracutaneous testing evaluates cytotoxicity reactions at the deepest skin level. Thus, intracutaneous testing might evaluate plastics used in surgical equipment that interact with deep skin tissues for short periods.
Summary
Overall, cytotoxicity testing evaluates the toxicity of the polymeric materials used by medical devices and products. This article compares three in-vitro cytotoxicity tests from USP 87 (direct contact, agar diffusion, and elution testing). Additionally, three cytotoxicity tests in live animals from USP 88 are compared. These in-vivo tests are implantation, intracutaneous injection, and systemic injection studies. Only in-vitro (benchtop) testing will be necessary to evaluate cytotoxicity in most circumstances. The types of cytotoxicity testing to perform for your medical device or product depend upon the final product’s construction, intended use, and packaging materials. All in all, ensure you choose a contract testing organization that can support you with appropriate cytotoxicity testing for your unique medical device or product needs.
Ethide Labs is a contract testing organization specializing in Cytotoxicity Testing. Ethide Labs also offers Microbiology Testing, Bioburden Testing, EO Residual Testing, Bacterial Endotoxin Testing, Sterility Testing, Environmental Monitoring & Package Integrity Testing services for medical device companies and allied industries. Ethide is an ISO 13485 certified facility.
References
Michael J. Akers. Sterile Drug Products Formulation, Packaging, Manufacture, and Quality. Drugs and the Pharmaceutical Sciences. Informa Healthcare. 2010.
United States Pharmacopeial Convention. <87> Biological Reactivity Tests, In Vitro. Rockville, MD, USA. 2021. (USPC <87>).
United States Pharmacopeial Convention. <88> Biological Reactivity Tests, In Vivo. Rockville, MD, USA. 2021. (USPC <88>).
Share this in your social networks


