Top 7 Sources Of Microbial Contamination
What is sterilization?
Sterilization is any process that removes, kills, or deactivates all forms of life. Sterilization is related to the term sterile, which means a complete absence of viable microorganisms or viruses that have the potential to reproduce. Thus, sterile products that undergo sterilization are often chemical (ethylene oxide gas), heat (steam or dry heat), or radiation sterilized. Sterilization kills any microorganisms (including resistant bacterial spores) inside the products obtained during manufacturing. Sterilization occurs after the product is placed in its final packaging for gas, heat, or radiation sterilization. The last sterilization process after manufacturing is known as terminal sterilization.
There are four main methods that sterilize items:
- Heat
- Gas
- Radiation
- Filtration
Another way to classify these four sterilization methods is:
What is sanitization?
Sanitization reduces the microbial population. However, unlike sterilization, sanitization does not aim to eliminate the microbial population by a specific amount.
Which microorganisms do sterilization and sanitization processes eliminate?
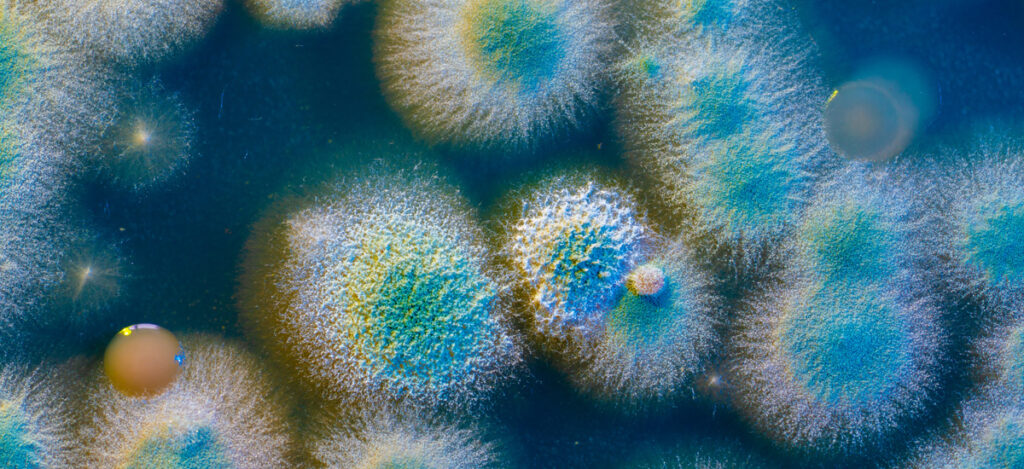
Sanitization and sterilization processes reduce or eliminate three primary microbe types: bacteria, fungi (yeast and mold), and viruses.
What are the sources of microbial contamination?
For microbial contamination to occur, microbes must be present, and the microbes must be in an environment that supports their growth. Indeed, microorganisms must have appropriate nutrients, humidity, and temperature to grow. Food sources for microorganisms are organic or proteinaceous materials. Microbial moisture requirements can be met with both relative humidity in the environment and any water sources. Microorganisms are capable of surviving a wide range of temperatures, especially fungi. However, room temperature is the gold standard for microbial growth. A microbe that falls into an environment where it cannot survive and multiply will die. Below we describe the top seven microbial contamination sources for medical devices and medical products. These contamination sources should be controlled using appropriate aseptic environmental monitoring or non-sterile environmental monitoring techniques.
#1: People
People are the greatest source of microbial contamination. Product contamination risk is almost entirely related to human activity. Microbes live all over the human body in our skin, hair, clothing, and moisture droplets from our breath. Anything humans touch, shed (think flakes of skin or hair), breath on, cough on, or brush up against is a source of microbial contamination. Movements as simple as walking can emit more than 10,000 particles per minute. While protective gear like gloves, gowns, masks, and booties help with microbial contamination. The more human interaction during manufacturing can be limited, the lower the risk of microbial contamination.
#2: Water
Other than people, water is the number one source of microbial contamination. Microorganisms readily exist and multiply in water. Thus, using sterile water during product processing flushes and equipment cleaning is critical to prevent unwanted microbial contamination. Water control is crucial to cleanroom success. Microorganisms that are native to fresh water and ubiquitously found there include Pseudomonas sp., Bacillus sp., and Escherichia coli. Bacillus sp. is commonly washed into the water during rainfall. Escherichia coli comes from sewage contaminants in the water supply. Water sampling methods can be used to monitor water contaminants.
#3: Raw Materials
Most raw materials come from plants or animal sources. Thus, raw materials can be contaminated with pathogens such as E. coli and Salmonella. Even synthetic raw materials (in contact with humans during production) are subject to contamination if they are not produced under aseptic conditions. Molds are also of issue, especially for raw materials that have undergone long-term storage in humid environments.
#4: Packaging
Plastic materials have relatively low-surface microbial contamination. However, any rubber closures or paper (such as cardboard containers) are excellent homes for mold growth. Even glass can support mold spore growth (such as Penicillin and Aspergillus) or the growth of some bacteria (such as Bacillus). Thus, appropriate packaging and storage conditions are essential to preventing microbial contamination of products.
#5: Buildings
Walls and ceilings for manufacturing and storage buildings can contain molds, such as Cladosporium sp and Aspergillus sp. The plaster that paints cover is a source of nutrients for microbes. Contamination risks for walls, ceilings, or floors occur if water is present in any cracks, sealing, edges, or joints. Disinfectant-resistant biofilms will quickly develop in these areas of the building if moisture is present.
#6: Equipment
Hard-to-clean equipment locations are harbors for microbial contamination. Such locations are often small and patterned. Some examples of difficult-to-clean areas are screw threads, agitator blades, valves, and pipe joints. Note that cleaning equipment (sponges, brooms, and mops) can become sources of contamination if not sterilized or replaced regularly.
#7: The Atmosphere
While air is too dry and clean (nutrient-free) to support microbial growth, microorganisms can still survive in the air for brief periods until they land on surfaces that can support their survival and growth. Thus, microorganisms use air as a vehicle for transportation more than an environment for growth. The organisms that tolerate a dry climate best include Bacillus, Clostridium, Staphylococcus, Streptococcus, Penicillin, Aspergillus, and Rhodotorula. The degree of airborne contaminants in an environment depends on the relative levels of dust, particles, and humidity. The higher the dust, particulate, or humidity levels, the greater the risk of viable airborne contaminants. Air sampling can be utilized to monitor airborne contaminants.
Summary
Overall, sterilization is any process that removes, kills, or deactivates all forms of life. Sterilization for medical devices and products is critical for ensuring patient safety during product use. There are three primary microbe types that require appropriate elimination before medical product usage: bacteria, fungi (yeast and mold), and viruses. The easiest way to eliminate microbes is to prevent microbial contamination altogether. To this end, the top seven sources for microbial contamination of medical devices and products are people, water, raw materials, packaging, buildings, equipment, and air. Ultimately, minimizing human and water-based contaminants is the top way to prevent microbial contamination of a medical product or device. All in all, as you navigate medical product manufacturing, ensure you choose a contract testing organization that can support you with appropriate environmental monitoring, microbiology testing, and sterilization validations for your unique medical device or product needs.
Ethide Labs is a contract testing organization specializing in Microbiology Testing & Cytotoxicity Testing. Ethide Labs also offers Bacterial Endotoxin Testing, EO Residual Testing, Environmental Monitoring, Sterility Testing, Bioburden Testing & Package Integrity Testing services for medical device companies and allied industries. Ethide is an ISO 13485 certified facility.
References
International Organization for Standardization. Sterilization of health care products- Moist heat- Part 1: Requirements for the development, validation, and routine control of a sterilization process for medical devices. Geneva (Switzerland): ISO; 2006. (ISO 17665-1:2006/(R)2016).
Michael J. Akers. Sterile Drug Products Formulation, Packaging, Manufacture, and Quality. Drugs and the Pharmaceutical Sciences. Informa Healthcare. 2010.
United States Pharmacopeial Convention. <1115> Bioburden Control of Non-Sterile Drug Substances and Products. Rockville, MD, USA. 2021. (USPC <1115>).
United States Pharmacopeial Convention. <1116> Microbiological Control & Monitoring of Aseptic Processing Environments. Rockville, MD, USA. 2021. (USPC <1116>).
United States Pharmacopeial Convention. <1211> Sterility Assurance. Rockville, MD, USA. 2021. (USPC <1211>).
Share this in your social networks


