Top Biological Indicators For Each Sterilization Validation Process
What is sterilization?
Sterilization is any process that removes, kills, or deactivates all forms of life. Sterilization is related to the term sterile, which means a complete absence of viable microorganisms or viruses that have the potential to reproduce. Thus, sterile products that undergo sterilization are often chemical (gas), heat, or radiation sterilized. Sterilization kills any microorganisms inside the products obtained during manufacturing. Sterilization occurs after the product is placed in its final packaging for gas, heat, or radiation sterilization. The last sterilization process after manufacturing is known as terminal sterilization.
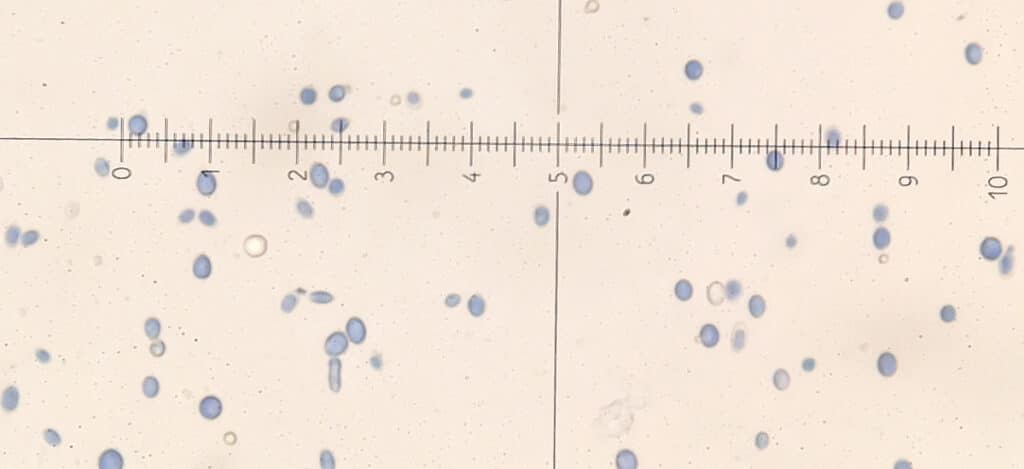
What is a biological indicator?
A biological indicator (BI) is a preparation of one or more spore-forming microorganisms that have resistance to being killed during sterilization. The spore-forming microorganisms used in biological indicators are well characterized and selected based on the sterilization process being tested. Spore-forming microorganisms (gram-positive bacteria) are used as BIs because they are exponentially more difficult to kill during sterilization than non-spore-forming microbes or spore-forming microbes in an active state. Furthermore, spore-forming microbes represent a minimal subset of the actual bioburden on items to be sterilized. Thus, if a sterilization process can destroy the bioburden of a product represented entirely as spores, the sterilization process will be able to kill all microbes in a “worst-case” bioburden situation. The biological indicator’s ability to mimic “worst-case” bioburden scenarios is how BIs validate sterilization processes and prove that a process is effective enough to sterilize a product in its final package consistently. Other common sterilization processes validated with BIs are the sterilization of manufacturing equipment and packaging components. BIs are also used to monitor and reassess sterilization processes for their effectiveness periodically.
What types of biological indicators are there?
Some BIs contain a single microorganism species, while others contain two species and concentrations of bacterial spores to compare different sterilization processes. There are three primary types of BI indicators.
#1: Spores on a carrier
In this preparation, spores are placed on a carrier (e.g., a disk or strip). The disks or strips can be paper, glass, plastic, metal, or other materials. BI’s using a carrier are often packaged to maintain the integrity and viability of the inoculated spores on the carrier. Following sterilization, neither the BI carrier nor the BI packaging should be damaged or degraded.
#2: Spore suspension
Biological indicators can also be an inoculate spore suspension placed on the product being sterilized or into representative units of the product to be sterilized. A surrogate article that is substantially similar to the product being sterilized can be used if it is not practical to inoculate the actual product. For spore suspensions used in liquid products, the population and D value of the BI spore is critical to determine to evaluate the efficiency of the sterilization process.
#3: Sealed system spores
The third BI option is a sealed system. This sealed system includes the growth medium and the BI microorganisms. The growth medium is either in direct contact with the BI species during the sterilization or is placed in contact with the BI after sterilization. The growth media supports the recovery of any sterilization process-exposed BI microorganisms. Some BI systems contain a growth indicator or sensor in addition to growth media.
Which biological indicators should be used for each sterilization process?
Biological indicator selection is based on the resistance of the BI to the sterilization process. The BI system must provide a greater challenge to the sterilization process than the native bioburden of the product being sterilized. The biological indicator suggestions by sterilization process below represent the most common choices. However, other biological indicators may be used with appropriate justification. Overall, the typical BIs are spore-forming bacteria of the genera Geobacillus, Bacillus, and Clostridium.
Moist Heat Sterilization (Steam Sterilization) by Direct Contact
Moist heat sterilization of most non-liquid products is known as steam sterilization by direct contact. Steam sterilization traditionally uses spores of G. stearothermophilus as a BI. G. stearothermophilus is a microorganism that likes heat that has a moist heat resistance substantially greater than that of most active microorganisms. Note that active microorganisms are organisms not in their spore form.
Moist Heat Sterilization of Aqueous Liquids
For moist heat sterilization, heat-resistant spore-forming microorganisms such as C. sporogenes, B. subtilis, or B. atrophaeus are chosen as biological indicators. These spore-forming microorganisms are also preferred for verifying the sterilization of aqueous solutions due to their lower thermal resistance.
Dry Heat Sterilization
Spores of B. atrophaeus are typically used for dry heat sterilization. Note that the temperatures needed to depyrogenate materials are more than sufficient to sterilize them. Thus, if dry heat depyrogenation has been demonstrated, sterilization by dry heat does not need to be confirmed, and a BI is not required.
Ionizing Radiation
A resistant biological indicator isn’t needed to evaluate radiation sterilization processes. Radiation dose settings will need to know pre-irradiation bioburden. Radiation methods can be verified using dosimetric evaluations.
Gas Sterilization
Spores of B. atrophaeus are traditionally used for verification of ethylene oxide sterilization processes. For other gases, spores of G. stearothermophilus or B. atrophaeus are often used as BIs.
Chemical Sterilization
For sterilization by a liquid sterilant, spores of B. atrophaeus, B. subtilis, or another similar spore-forming species are used as biological indicators. As for all other sterilization processes, the BI strain should have greater resistance to the sterilization process than the product’s native bioburden.
Vapor Phase Sterilization
Either G. stearothermophilus or B. atrophaeus can be used to evaluate vapor phase sterilization processes.
Summary
Overall, sterilization is any process that removes, kills, or deactivates all forms of life. Most medical devices, parenteral products, and other health care items must be sterile to be used by a patient. Sterilization processes for healthcare products are validated using biological indicators (BIs). A biological indicator is a preparation of one or more spore-forming microorganisms that have resistance to being killed during sterilization. Typical BIs are bacteria of the genera Geobacillus, Bacillus, and Clostridium. When selecting a BI for sterilization validation, the BI strain should have greater resistance to the sterilization process than the product’s native bioburden. Traditional BI strains for each sterilization process are detailed in the article above. All in all, ensure you choose a contract testing organization that can provide appropriate sterilization validations for your product needs.
Ethide Labs is a contract testing organization specializing in Sterilization Validations & Sterility Testing. Ethide Labs also offers Microbiology Testing, Bacterial Endotoxin Testing, EO Residual Testing, Environmental Monitoring, Cytotoxicity Testing, Bioburden Testing & Package Integrity Testing services for medical device companies and allied industries. Ethide is an ISO 13485 certified facility.
References
International Organization for Standardization. Sterilization of health care products- Moist heat- Part 1: Requirements for the development, validation, and routine control of a sterilization process for medical devices. Geneva (Switzerland): ISO; 2006. (ISO 17665-1:2006/(R)2016).
Michael J. Akers. Sterile Drug Products Formulation, Packaging, Manufacture, and Quality. Drugs and the Pharmaceutical Sciences. Informa Healthcare. 2010.
United States Pharmacopeial Convention. <1229.5> Biological Indicators For Sterilization. Rockville, MD, USA. 2021.(USPC <1229.5>).
United States Pharmacopeial Convention. <1115> Bioburden Control of Non-Sterile Drug Substances and Products. Rockville, MD, USA. 2021. (USPC <1115>).
United States Pharmacopeial Convention. <1116> Microbiological Control & Monitoring of Aseptic Processing Environments. Rockville, MD, USA. 2021. (USPC <1116>).
United States Pharmacopeial Convention. <1211> Sterility Assurance. Rockville, MD, USA. 2021. (USPC <1211>).
Share this in your social networks


