Subvisible Particle Detection Within Traditional Parenteral Products vs. Therapeutic Protein Biologics
What is particulate matter testing, and what test methods are available?
Particulate matter refers to undissolved particles (other than gas bubbles) that are present in solutions. This particulate matter is not an intentional addition to a parenteral product, and parenteral products are to be free from particles that can be visually observed. Just as unintentional microbes in injectables are avoided and regulated to prevent patient illness, unintentional and non-biological particles are regulated in products to avoid unwanted toxicity, illness, or side effects.
Particulate matter can be detected in two ways: a light-obscuration particle count test and a microscopic particle count test. Light-obscuration particle count testing is preferred for subvisible particle detection for both traditional parenteral products and biologics. However, traditional parenteral preparations with reduced clarity or increased viscosity (such as emulsions, colloids, and liposomal formulations) should be assessed using microscopic particle count testing. Microscopic particle count testing cannot give accurate results for protein biologics. Thus, microscopic particle count tests can be used to confirm intrinsic vs. extrinsic particles for biologics only. In some cases, both particulate matter test methods will be needed to confirm subvisible particle counts for traditional parenteral products. In instances where the viscosity of the test preparation is high, a quantitative dilution with an appropriate diluent may be made to decrease viscosity, as necessary, to allow the particulate analysis to be performed.
How is particulate matter testing different for therapeutic protein products?
Therapeutic protein injections are products containing proteins or peptides. Particulate matter in therapeutic protein injections may be (a) truly foreign, or “extrinsic,” e.g., unexpected foreign material, such as cellulose; (b) “intrinsic” resulting from an unexpected addition into the product such as dust due to insufficient cleaning during manufacturing; and (c) “inherent,” such the protein or formulation components themselves. All these particle types are detected and counted for therapeutic protein injectables.
The light-obscuration particle count test is the most accurate method for therapeutic protein injection subvisible particle evaluation. Microscopic particle count testing can be used to differentiate intrinsic vs. extrinsic particles but cannot be used for the particle count for therapeutic protein products itself.
How is light obscuration testing of therapeutic protein injections and traditional parenteral products performed?
Light-obscuration particulate matter testing uses a liquid particle counter machine that, based on the principle of light scattering, allows for an automated determination of the size of particles in a sample and the number of particles according to size. The liquid particle counter is calibrated using dispersions of spherical particles in particle-free water. The liquid particle counter will have a sensor capable of detecting particles within the anticipated particle size range and particle count volume. For traditional parenteral product tests detailed in USP 788, particles are of known sizes between 10 microns (μm), and 25 μm are identified. For therapeutic proteins, particles often range from 2 μm to 100 μm.
For testing of traditional parenteral products, each sample’s contents are mixed by slow inversion. Care is taken not to introduce air bubbles into examined preparations. Gas bubbles are further eliminated by allowing samples to stand for 2 minutes after inversion or through sonication. For small-volume Parenterals (less than 25 milliliters in volume), the contents of 10 or more units are combined in a cleaned container to obtain a volume not less than 25 milliliters (mL). Powders for parenteral use are reconstituted with particle-free water or with an appropriate particle-free solvent when particle-free water is not suitable. Injectables with a volume of 25 mL or more are tested individually. For pharmacy bulk packages “Not for Direct Infusion,” calculate the test result on a portion equivalent to the maximum labeled dose. For example, if the average particle count per mL is 5, you would multiply the particle count per mL by 10 to obtain the particle count for the 10-mL maximum dose. In this example, the particle count for the 10-mL maximum dose is 50. Products meant to hold a drug product and a solvent should be tested as directed for large-volume parenterals or small-volume parenterals, depending on container volume. The number of samples must be adequate to provide a statistically sound assessment. Less than ten individual units may be tested for parenterals with a volume of 25 mL or more. After careful mixing, remove four aliquots, no less than 5 mL each, and count the number of particles equal to or greater than 10 μm and 25 μm.
For therapeutic protein biologics, a single test requires 0.2–5.0 milliliters (mL) of product. Product samples are pooled to generate the appropriate testing volume if needed. If a product requires reconstruction, the reconstitution or dilution must be performed with the proper amount of specified solvent. Subtraction of the solvent particle count from the total particle count is not allowed. The reconstituted products must meet therapeutic protein particle count requirements with their respective solvents included. Under certain circumstances, such as with high-concentration products that could saturate the particle counter instrument sensor or high-viscosity products, a dilution of the product samples may be performed to obtain reliable results. If dilution is needed, additional studies exploring the effect of dilution on particle aggregates or changes in the protein ratio to excipients should be performed. Care should be taken to minimize shaking, inversion, sonication, and other stresses to the product samples to prevent the introduction of air bubbles. Any air bubbles in the samples will result in false-positive particle results. Air bubbles can be further eliminated by allowing the product to rest under ambient pressure or by applying a gentle vacuum to the samples. Samples should undergo a slow mixing (such as swirling the container by hand) before four aliquots of the product are evaluated in the particle counter.

What are the light-obscuration method limits for therapeutic protein injection particle counts?
Once particles have been counted, acquire the number of particles over the selected size range, including particles equal to or greater than 10 and 25 μm. For infusion or injections with a volume of less than or equal to 100 mL, the average number of particles present in the units tested should not exceed 6000 particles per container equal to or greater than 10 μm, and not exceed 600 particles per container equal to or greater than 25 μm. For therapeutic protein injections/infusions greater than 100 mL, the average number of particles in the units tested should not exceed 25 particles per mL equal to or greater than 10 μm and should not exceed 3 particles per mL equal to or greater than 25 μm. Additionally, with product volumes greater than 100 mL, the total particle load should meet the same limits as the particle load for products less than or equal to 100mL. In other words, the total particle load should not exceed 6000 particles per container equal to or greater than 10 μm and should not exceed 600 particles per container equal to or greater than 25 μm. For products first reconstituted in less than 100 mL and then diluted for infusion in a volume greater than 100 mL, particle content should be assessed both before and after dilution and evaluated based on their final volume.
What are the light-obscuration method limits for all other parenteral products particle counts?
Once particles have been counted, calculate the mean number of particles for the sample examined. For light obscuration particle count tests, there are two test criteria. For sample preparations with a volume of more than 100 mL, the first test criteria apply. Samples with a volume of fewer than 100 mL use the second test criteria. In the first test criteria, the sample complies with the particle count test if the average number of particles present in the units tested does not exceed 25 particles per mL equal to or greater than 10 μm and does not exceed 3 particles per mL equal to or greater than 25 μm. In the second test criteria, the sample meets the test criteria if the average number of particles tested does not exceed 6000 particles per container equal to or greater than 10 μm and does not exceed 600 particles per container equal to or greater than 25 μm. If the average number of particles exceeds the limits, test the parenterals by the microscopic particle count test.
How is microscopic particle count testing of parenteral products performed?
The light obscuration method is the preferred method for therapeutic protein injections and parenteral infusions. For actual particle count testing, the light-obscuration method should be used. However, the microscopic method may be used to determine extrinsic and intrinsic particle types. Note that the microscopic particle count test results are not equivalent to those of the light-obscuration particle count test. Test results are not comparable because of differences in interference of some protein particles due to their fragile or translucent nature. Thus, you cannot interchange these two methods for the determination of extrinsic and intrinsic particle types.
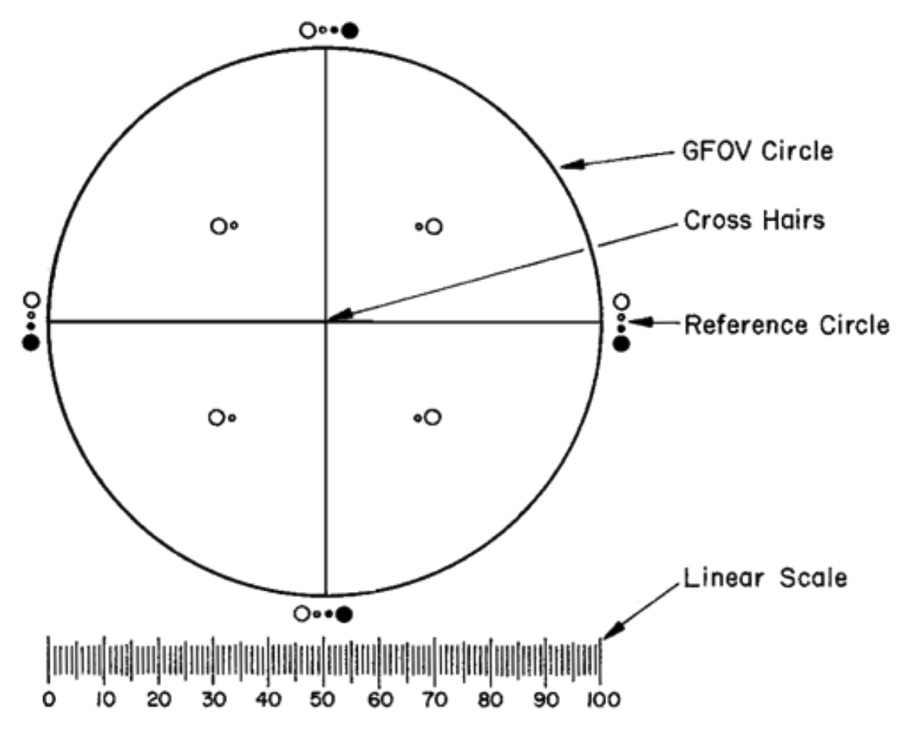
Microscopic particle count testing uses a binocular microscope, a filter assembly for retaining particulate matter, and a membrane filter for sample examination for parenteral products. The microscope will have an ocular micrometer with a graticule (see Figure 1 reproduced from Figure 1 of USP 788 below). The ocular micrometer is calibrated using a stage micrometer certified by either a domestic or international standard institution. Additionally, two illuminators (one internal and one external) are needed for the microscope assembly.
For testing, each sample’s contents are mixed by slow inversion. For small-volume parenterals (less than 25 milliliters in volume), the contents of 10 or more units are combined in a cleaned container to obtain a volume not less than 25 milliliters (mL). If a powder for parenteral use is tested, the powder is reconstituted with particle-free water or an appropriate particle-free solvent to ensure test accuracy. Injectables with a volume of 25 mL or more do not need to be pooled and are tested individually. Overall, the number of samples (pooled or not) must be adequate to provide a statistically sound assessment.
What are the microscopic particle count method limits for parenteral products that are not protein therapeutics?
For traditional parenteral products, the mean number of particles for the sample examined is calculated once the particles have been counted. For microscopic particle count tests, there are two test criteria. For sample preparations with a volume of more than 100 mL, the first test criteria apply. Samples with a volume of fewer than 100 mL use the second test criteria. In the first test criteria, the sample complies with the particle count test if the average number of particles present does not exceed 12 particles per mL equal to or greater than 10 μm and does not exceed 2 particles per mL equal to or greater than 25 μm. The sample meets the testing criteria in the second test criteria if the average number of particles present in the units tested does not exceed 3000 per container equal to or greater than 10 μm and does not exceed 300 per container equal to or greater than 25 μm.
Summary
Overall, particulate matter testing is an important microbiology test for parenteral products. Therapeutic protein biologics have some additional requirements for particle count testing due to the combination of extrinsic, intrinsic, and inherent particles within these products. Unintentional, non-biological particles are regulated in protein therapeutic and other parenteral product formulations to prevent unwanted toxicity, illness, or side effects in patients following treatment. Two tests are traditionally used for particulate matter testing: a light-obscuration particle count test and a microscopic particle count test. The light obscuration particle count method is used for all therapeutic protein particle count tests for accurate particle detection. Microscopic particle count testing can be used for other parenteral products and should only be used for biologics to verify intrinsic and extrinsic particle types. All in all, when developing your therapeutic protein product, ensure you choose a contract testing organization that can support you with appropriate microbiology particle count testing for your unique product needs.
Ethide Labs is a contract testing organization specializing in Particulate Matter Testing and Microbiology Testing. Ethide Labs also offers EO Residual Testing, Sterility Testing, Cytotoxicity Testing, Bacterial Endotoxin Testing, Bioburden Testing, Package Integrity Testing & Environmental Monitoring services for medical device companies and allied industries. Ethide is an ISO 13485 certified facility.
References
United States Pharmacopeial Convention. <787> Subvisible Particulate Matter In Therapeutic Protein Injections, In Vitro. Rockville, MD, USA. 2021. (USPC <787>).
United States Pharmacopeial Convention. <788> Particulate Matter In Injections, In Vitro. Rockville, MD, USA. 2021. (USPC <788>).
Share this in your social networks


