Radiation Sterilization Vs. Vapor Sterilization
What is sterilization, and why is it essential for sterile products?
Sterilization keeps patients safe from toxins and microbial illnesses when therapies or devices are consumed or used. Sterilization is any process that removes, kills, or deactivates all forms of life. Under the strictest definition of sterility, an item or product is sterile when there is the complete absence of viable microorganisms (bacteria, yeasts, viruses, and molds). For regulatory purposes, sterility is defined by acceptance criteria based on calculated contamination probability. An acceptable level of contamination risk for most items is the probability of a single contaminated product out of a million manufactured products. However, sterility criteria may be more stringent or lax depending upon the intended use of the medical device or product. Commonly, sterile products undergo sterilization processes that utilize chemicals, heat, radiation, or filters. Sterilization kills any microorganisms products collect during manufacturing. A less common version of sterilization is vapor phase sterilization. Chemical vapor sterilization (like hydrogen peroxide vapor sterilization), medical radiation sterilization, radiation sterilization processes, and chemical vapor sterilization uses will be covered in this article. Note that chemical vapor sterilization uses are limited.
What is radiation sterilization (sterilization by radiation)?
Sterilization by radiation is a non-thermal sterilization method that functions by destroying any microorganisms in a product with gamma radiation, beta particles (electron beam), x-ray, or ultraviolet (UV) light. Other than sterile filtration, sterilization by radiation is the only other sterilization method that doesn’t rely on elevated temperature to sterilize. Sterilization by radiation is an excellent alternative for products that cannot be sterilized with heat or chemicals.
What is vapor phase sterilization?
Vapor is an agent or molecule that is suspended in the air. Vapor phase sterilization sterilizes products through exposure to sporicidal agents suspended in the air. Traditional chemical vapor sterilization uses use hydrogen peroxide (H2O2), peracetic acid (CH3CO3CH), formaldehyde (CH2O), and glutaraldehyde [CH2(CH2CHO)2] as sterilization agents. Sterilizing gases and liquids differ from vapor phase agents, as vapor phase agents expose products to multiple phases (liquid, gas, etc.) during sterilization.
What items can be sterilized by radiation?
Items sterilized with radiation are the same as items that gaseous methods can sterilize. Standard devices and materials sterilized with radiation are plastics, heat-labile materials, glass, and powders. Radiation damages the nucleoproteins of microorganisms and thus is not recommended for biologics.
What products or medical devices can undergo vapor phase sterilization?
Chemical vapor sterilization uses are for the sterilization of heat-sensitive materials and the sterilization of surfaces. As mentioned above, chemical vapor sterilization uses are limited due to limited penetration and a material’s compatibility with hydrogen peroxide vapor.
How is Medical radiation Sterilization performed?
Simply speaking, medical radiation sterilization is performed by exposing a product to gamma radiation, beta particles, or ultraviolet light. Microwave radiation is sometimes used for empty glass containers but is not considered a primary radiation sterilization method. Electromagnetic gamma radiation is the most effective medical radiation sterilization method due to its deep penetration. Often cobalt 60 high-energy photons are used for gamma radiation. Beta particles, as ionizing radiations, are not electromagnetic and less penetrative. Mechanically accelerated Strontium 90 creates exceptionally high energy levels and the beta particles (electron beams) needed for beta particle radiation. Ultraviolet light can also be used but only as a surface sterilizing method. The energy level of ultraviolet light is too weak to penetrate materials. Gamma sterilization is the most robust option for radiation sterilization, but beta particle (e-beam) radiation is also used for product terminal sterilization.
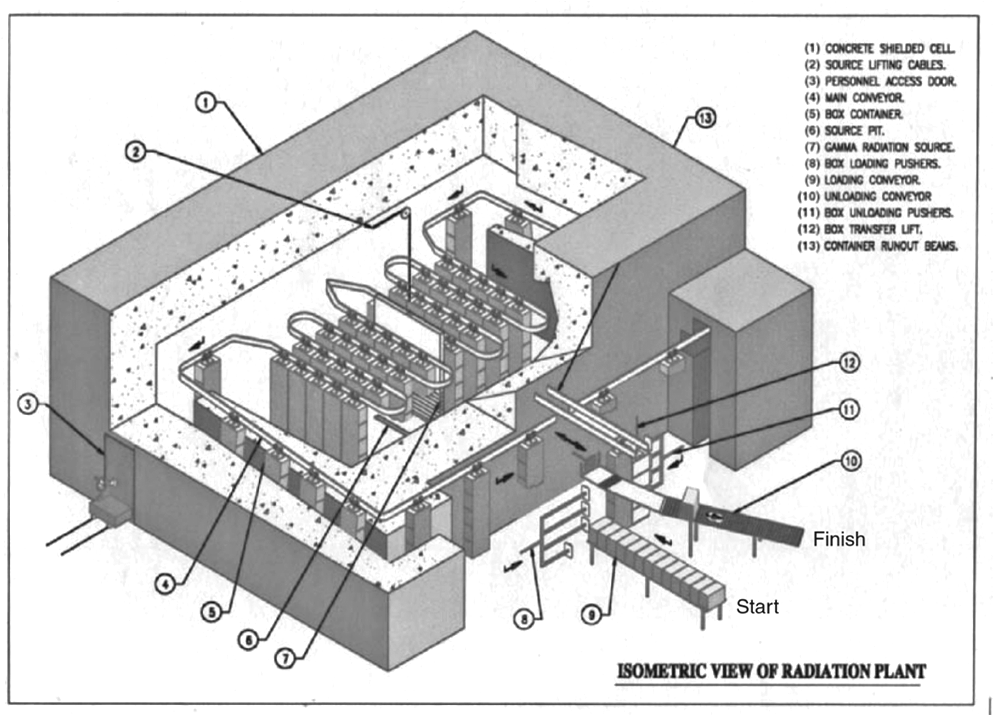
Radiation effectiveness is dependent on the medical radiation sterilization dosage and time exposure. A 12-D sterilization overkill approach is used in radiation sterilization. The 12-D stands for providing a radiation dose sufficient to produce a 12-log reduction in the D value of the most resistant microbial spore. Note that D value determination for radiation uses dosage rather than time. Typical D values for the most resistant bacterial spore (Bacillus pumulis) to radiation is 1.7 to 2.0 megarad (mRad). Commonly a radiation dosage will be 25 mRad, greater than 12-fold the D value of B. pumulis. During radiation sterilization treatment, dosimeters are placed at strategic locations to monitor radiation doses products receive throughout the sterilization process. When a product goes through a radiation sterilization conveyor (see Figure 1 below), the total radiation dosage is unequally distributed as items under sterilization are conveyed from start to finish. Total radiation percentages are greatest in conveyor areas closest to the gamma radiation source. The total radiation dose for sterilization experienced by a product may be 25 mRad. The total radiation dosage is distributed throughout the conveyor system to avoid applying an overwhelming or damaging amount of radiation at any given time during sterilization.
Factors that affect Medical radiation sterilization:
- D value of the biological indicator or bioburden level of the item undergoing sterilization
- Radiation strength
- Radiation dose rate
- Conveyor speed
How is vapor phase sterilization performed?
At room temperature, vapor phase agents (liquids or solids) vaporize and can be utilized for sterilization within a sealed chamber or vessel. Vapor sterilization must have a correct sterilant concentration, chamber temperature, and relative humidity for the items undergoing sterilization. Typically, the sterilant concentration (amount) will be determined from its injection quantities into the sterilization chamber. Vapor phase agents are most often introduced as an aqueous solution. For example, a standard vapor sterilization process involves adding items into the sterilization chamber and then adding heat and humidity. Next, the sterilant agent is introduced (sometimes through an atomizer), and the products are marinated in the vaporized sterilant for a set time. And finally, allowing the vapor to be removed from the system or evaporate before opening the chamber and removing the newly sterile items. If introduced as an aqueous solution, water moisture is introduced along with the sterilant. This added moisture is factored into humidity and condensation considerations for the sterilization process. Out of all vapor phase agents, hydrogen peroxide and peracetic acid are widely used and the most established for sterilization.
Hydrogen Peroxide Vapor Phase Sterilization
Hydrogen peroxide has a long history of being a liquid sterilant in healthcare and other industries. Hydrogen peroxide can be added into a sterilization chamber through multiple approaches. These approaches are continuous administration, intermittent administration, or injecting the entire dose of hydrogen peroxide all at once. Some vapor phase sterilization protocols have a drying step before adding the hydrogen peroxide. This drying step allows the hydrogen peroxide concentration within the sterilization chamber to increase without additional condensation. Hydrogen peroxide can also be introduced to a chamber as a liquid and exposed to targeted heating to create the vapor phase. Like gaseous sterilization methods, the sterilization chamber is aerated, and the sterilant gas is allowed to dissipate before the sterilized medical devices, products, and other items are removed.
Peracetic Acid Vapor Phase Sterilization
Peracetic acid may be used alone or mixed with hydrogen peroxide to sterilize medical products and devices. Peracetic acid is a liquid sterilant. An atomizer is used to distribute peracetic acid for vapor phase sterilization. The atomizer allows both liquid and vapor forms of peracetic acid to be present during sterilization. After peracetic acid exposure, evaporation is used to remove all peracetic acid from the system.

What are the problems with radiation sterilization?
There is limited understanding of the molecular transformations in drug molecules and excipients under high-energy gamma radiation exposure. Additionally, there are not many gamma radiation or e-beam radiation sterilization centers available for bulk sterilizing products compared to other methods, such as ethylene oxide gas. Furthermore, a concern when sterilizing finished products or active pharmaceutical ingredients (APIs) with radiation is the risk of radiolytic byproduct formation (e.g., *OH) that could cause damage to the raw material, API, or product packaging system.
What are some difficulties with vapor sterilization?
Vapor phase sterilization can be challenging to validate as relative humidity, sterilant concentration, and condensation rate varies throughout the sterilization process. These variations cause localized differences in sterile conditions within a sterilization chamber. Thus, some products or product areas may not experience the same microbial lethality as other products or product parts. Further, there is no standardized biological indicator for vapor systems as it is a liquid and a gas combined sterilization system. D-values (which determine the lethality of a sterilization process) can be tricky to calculate for vapor sterilization systems because gas-phase conditions, surface conditions, and microbial lethality do not have known correlations. D-values can only be calculated under well-defined, system-to-system specific conditions.
What are the primary differences between using radiation vs. vapor sterilization?
Radiation and vapor sterilization are alternatives to traditional heat sterilization processes. The depth of radiation sterilization depends upon the type of radiation used. Gamma radiation has the deepest penetration into inner surfaces. Vapor sterilization is useful mostly for surface-level sterilization but can provide sterilization to some inner surfaces. Radiation sterilization does not work with materials that break down upon gamma, UV, or electron beam exposure. Gamma is the strongest of these radiation options and can cause the most material degeneration. In contrast, vapor sterilization does not work for materials that degrade upon exposure to peracetic acid or hydrogen peroxide sterilants. Neither sterilization method will work to sterilize products containing a biological agent.
Summary
Overall, medical devices, products, and therapies must be sterile. Sterilization is any process that removes, kills, or deactivates microbes. Radiation sterilization processes are cold sterilization methods that kill microbes through exposure to gamma, beta particle (e-beam), or ultraviolet radiation. In contrast, vapor sterilization inactivates microbes through exposure to sporicidal agents suspended in the air. Typical vapor phase sterilization agents are hydrogen peroxide, peracetic acid, formaldehyde, and glutaraldehyde. Radiation and vapor sterilization processes are alternatives to traditional heat sterilization methods.
Standard devices and materials sterilized with radiation are plastic materials, heat-labile materials, glass, and powders, whereas vapor sterilization works well for heat-sensitive materials compatible with peracetic acid or hydrogen peroxide exposure. All in all, ensure you choose a contract testing organization that can provide appropriate sterility testing for your product needs.
Ethide Labs is a contract testing organization specializing in Sterilization Validations and Sterility Testing. Ethide Labs also offers Microbiology Testing, Bioburden Testing, EO Residual Testing, Bacterial Endotoxin Testing, Cytotoxicity Testing, Environmental Monitoring & Package Integrity Testing services for medical device companies and allied industries. Ethide is an ISO 13485 certified facility.
References
Michael J. Akers. Sterile Drug Products Formulation, Packaging, Manufacture, and Quality. Drugs and the Pharmaceutical Sciences. Informa Healthcare. 2010.
United States Pharmacopeial Convention. <1116> Microbiological Control & Monitoring of Aseptic Processing Environments. Rockville, MD, USA. 2021. (USPC <1116>).
United States Pharmacopeial Convention. <1211> Sterility Assurance. Rockville, MD, USA. 2021. (USPC <1211>).
United States Pharmacopeial Convention. <1229> Sterilization of Compendial Articles. Rockville, MD, USA. 2021. (USPC <1229>).
United States Pharmacopeial Convention. <1229.10> Radiation Sterilization. Rockville, MD, USA. 2021. (USPC <1229.10>).
United States Pharmacopeial Convention. <1229.11> Vapor Phase Sterilization. Rockville, MD, USA. 2021. (USPC <1229.11>).
Share this in your social networks


